Dehydration Can Be Described as a Water Loss

Image : "The human body requires a minimum intake of water in order to be able to sustain life before balmy and then severe dehydration occurs." by Pan American Health Organisation. License: CC By-ND 2.0
Overview
Dehydration is defined as the excessive loss of water from the torso. The balance betwixt fluid intake and fluid loss from the trunk is greatly asymmetric in dehydration. The severity of dehydration ranges from balmy to severe, and dehydration can exist fatal when fluid loss exceeds more than 15% of the total body water.
Hypovolemia is defined as decreased circulatory volume due to blood or plasma loss.
Pathophysiology of Dehydration
Total trunk water is distributed into extracellular and intracellular compartments. The extracellular compartment contains ane-tertiary of total body water and consists of the intravascular, interstitial, and transcellular spaces. The intracellular compartment contains 2-thirds of the total body h2o and consists of the fluid inside the trunk's cells. In dehydration, fluid from the extracellular compartment is depleted first, followed by fluid from the intracellular space. Fluid loss from the intracellular space results in cellular shrinkage and metabolic dysfunction.
Aridity occurs because of decreased water intake, increased fluid loss, or both. In the elderly, impaired thirst sensation, chronic illness, fever, and sickness are mutual causes of decreased water intake. Common causes of increased fluid loss include vomiting, diarrhea, diuresis, and sweating. Working in hot weather without water and electrolyte replacement is another common cause of dehydration.
Dehydration tin be classified according to serum sodium concentration into hypernatremic, hyponatremic, or isonatremic dehydration.
- If h2o loss is greater in comparison to sodium loss, then the serum sodium concentration increases, resulting in hypernatremic (or hypertonic) dehydration.
- If water loss is accompanied by excessive sodium loss, then the serum sodium concentration decreases, resulting in hyponatremic (or hypotonic) dehydration.
- If water and sodium are lost at the same rate, then the serum sodium concentration remains the same. This is called isonatremic (or isotonic) aridity.
Apart from hypernatremia and hyponatremia, other electrolyte imbalances may also occur:
- Hyperkalemia, which occurs in insulin-dependent diabetes mellitus, Addison'south disease, and kidney failure.
- Hypokalemia, which results from increased potassium loss in severe diarrhea and vomiting.
- Hypermagnesemia and hyperphosphatemia can too occur from increased concentrations of magnesium and phosphate, respectively.
Evaluation of Total Torso Sodium
- Decreased total body sodium produces signs of volume depletion, including:
- Dry mucous membranes
- Decreased skin turgor (skin tenting when the skin is pinched)
- Decreased blood pressure and increased pulse (reflex tachycardia) when sitting up from the supine position (i.e., positive tilt test)
- Increased total body sodium may produce torso crenel effusions (ascites) and pitting edema.
- Dependent pitting edema is due to an excess of sodium-containing fluid in the interstitial space (over ii–3 L).
-
- Caused by low protein content in edematous fluid
- Fluid obeys the law of gravity and moves to the almost dependent portion of the body (ankles when standing).
-
- The Starling equation describes the forces that regulate the product of interstitial fluid; in the state of affairs of increased total body sodium. Starling pressures are altered to produce pitting edema and body effusions.
- An increase in total body sodium increases plasma hydrostatic pressure due to an increment in plasma volume.
- An increase in total torso sodium increases the weight of the patient and is the most common cause of weight gain in a hospitalized patient.
- Normal full body sodium is associated with normal skin turgor and hydration.
- Fluid movement across a capillary wall into the interstitial space is driven by Starling pressures (non osmosis).
- The net direction of fluid movement depends on which Starling force per unit area is ascendant.
- An increase in plasma hydrostatic pressure or a decrease in plasma oncotic force per unit area (i.e. serum albumin), causes fluid to diffuse out of capillaries and venules and into the interstitial space, resulting in dependent pitting edema and torso crenel effusions.
Signs and Symptoms of Dehydration
Nigh patients with dehydration present with:
- Thirst
- Headaches
- Fatigue
Symptoms of balmy dehydration include:
- Constipation
- Dry mouth
- Dizziness
- Depression urine volume (unless the cause of aridity is polyuria)
Symptoms of more astringent dehydration include:
- Dry skin
- Sunken optics
- Dry mucous membranes
- Defoliation
- Dizziness
- Hypotension
- Tachycardia
- Fever
- Poor skin elasticity
- Lethargy
- Oliguria
- Seizures
- Stupor
- Blackout
- Expiry
Signs of hypovolemia may also be present, including:
- Tachycardia
- Orthostatic hypotension
- Flat neck veins
Dehydration is more clinically evident in the elderly, especially in hot weather, due to impaired thirst sensation. Elderly or hospitalized patients volition testify signs of irritability and, occasionally, delirium.
Isotonic Dehydration
Isotonic dehydration is a condition in which both water and sodium are lost proportionally and the serum sodium concentration maintains normal serum osmolality. Serum osmolality determines the movement of fluids and electrolytes across membranes. The normal serum osmolality is 285–295 mOsm/kg.
Image: "Electron micrographs of viruses that crusade gastroenteritis in humans. A = Rotavirus (Rotavirus), B = Adenovirus (Adenoviridae), C = Norovirus (Norovirus) and D = Astrovirus (Astroviridae). They are shown at the aforementioned magnification of approximately ten 200,000" past Dr Graham Beards at en.wikipedia. License: CC BY three.0
Causes of isotonic dehydration
- Vomiting and diarrhea: severe watery diarrhea and vomiting can exist life-threatening atmospheric condition, especially in children. People with gastroenteritis may lose notable amounts of fluids and electrolytes within a curt time and their oral replacement is limited due to recurrent vomiting, which can upshot in severe dehydration.
- Excessive sweating: vigorous exercise, especially in humid atmospheric condition, will increase sweating and pb to fluid and electrolyte loss.
If dehydration is non corrected, it will lead to renal injury from musculus breakdown and lactic acidosis.
Laboratory values in isotonic dehydration
Isotonic aridity will show normal serum laboratory values, including normal osmolality (285–295 mOsm/kg) and normal serum sodium (135–145 mmol/L).
Urine volume will be decreased with low fractional sodium excretion and increased specific gravity.
Isotonic dehydration can event in elevated liver and pancreatic enzymes and a decreased glomerular filtration charge per unit. Dehydration also can result in various electrolyte imbalances that volition affect the clinical motion picture and prognosis.
Hypertonic Dehydration
Hypertonic dehydration occurs when water excretion from the body exceeds that of sodium excretion, resulting in increased sodium concentration in the extracellular fluid (hypernatremia). Blood osmolality is increased, causing water to shift from the intracellular to the extracellular space.
Causes of hypertonic dehydration
- Fever: Fever will increase the respiratory rate and therefore, water loss. Sweating also increases to lower the body temperature. Water intake is commonly decreased during a fever which will beal dehydration.
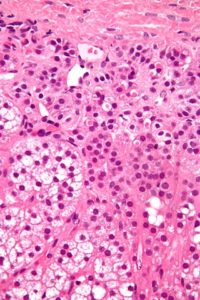
Image: "Micrograph of spironolactone bodies. H&E stain." by Nephron – Own work. License: CC BY-SA iii.0
- Polyuria: Increased water loss in the urine causes hypertonic dehydration and may occur in diabetes mellitus, diabetes insipidus, or with diuretic use.
- Decreased water intake
- Excessive sweating
- End-stage renal disease
- Drinking urine or seawater for survival
Laboratory values in hypertonic dehydration
Serum osmolality will exceed 300 mOsm/kg andserum sodium will exceed 150 mEq/L.
Urine volume will decrease unless the cause of aridity is polyuria or diuretic utilize.
Specific gravity will be high and partial excretion of sodium will also increase.
| Compartment Alteration | POsm/Na+ | ECF Volume | ICF Volume | Weather condition |
| Hyperglycemia | Increased glucose Decreased Na+ (dilutional event) | Contracted | Contracted |
|
| Hypertonic changes | ||||
| Hypotonic loss of Na+ | Decreased TBNa+ Decreased TBW | Contracted | Contracted |
|
| Loss of water | Increased TBNa+ Decreased TBW | Contracted (mild) Normal skin turgor | Contracted |
|
| Hypertonic gain of Na+ | Increased TBNa+ Increased TBW | Expanded | Contracted |
|
ECF, extracellular fluid; ICF, intracellular fluid; TBNa+, total trunk sodium; TBW, total trunk water
Hypotonic Dehydration
Hypotonic dehydration occurs when sodium loss is greater than h2o loss, resulting in a decrease in serum osmolality. This causes a shift of water from the extracellular space into the intracellular space. The cells swell and cerebral edema may occur.
Hyponatremia tin be acute or chronic. If sodium loss occurs for more than 48 hours, it becomes chronic hyponatremia, and the trunk may accommodate to this state. Sodium imbalance mainly manifests as neurological symptoms ranging from headaches, nausea, lethargy, and potentially confusion, coma, and death.
The term hyponatremia should be used with caution in cases of aridity, equally nearly cases of hyponatremia imply excess water retention rather than aridity.
Causes of hypotonic dehydration
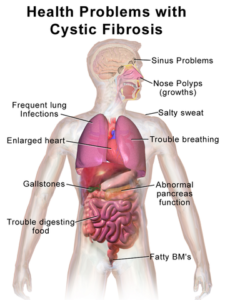
Image: "Health problems with cystic fibrosis" by Blausen.com staff. "Blausen gallery 2014". Wikiversity Journal of Medicine. DOI:10.15347/wjm/2014.010. License: CC BY three.0
- Addison'southward disease
- Renal tubular acidosis
- Iatrogenic causes: hypotonic fluids or regular saline used for 4 hydration in patients with heat stroke or diarrhea
- Diuretics: loop, thiazide, and osmotic diuretics, especially with prolonged utilize
- Cystic fibrosis
Laboratory values in hypotonic dehydration
Serum sodium and serum osmolality will exist less than the normal range.
Urine specific gravity will be decreased
Urine sodium excretion volition be decreased.
Isotonic and Hypotonic Fluid Disorders: Summary
| Compartment Alteration | POsm/Na+ | ECF Volume | ICF Volume | Conditions |
| Normal | Normal | Normal | Normal | |
| Isotonic and hypotonic changes | ||||
| Isotonic loss | Normal, ↓TBNa+/ ↓TBW | Contracted | Normal |
|
| Isotonic gain | Normal, ↑ TBNa+/ ↑TBW | Expanded | Normal |
|
| Hypertonic loss of Na+ | Decreased, ↓↓ TBNa+/ ↓TBW | Contracted | Expanded |
|
| Hypotonic gain of Na+ | Decreased, TBNa+/ ↑↑TBW | Expanded | Expanded |
|
| Decreased, ↑ TBNa+/ ↑↑TBW | Expanded Starling pressure alteration | Expanded |
| |
ECF, extracellular fluid; ICF, intracellular fluid; TBNa+, total body sodium; TBW, total trunk water
Complications of dehydration:
- Hypovolemic stupor: Severe dehydration will atomic number 82 to low claret volume and hypovolemic shock. It can atomic number 82 to major terminate-organ harm through acidosis and can cause acute kidney injury which tin can exist fatal.
- Seizures: Sodium imbalance can crusade abnormal neuronal excitability, resulting in confusion, seizures, delirium, and blackout. Seizures in dehydrated patients can exist iatrogenic or caused by the rapid correction of underlying serum sodium abnormalities. Hypotonic saline, if used in hypernatremic patients, will rapidly subtract the plasma osmolality and water will shift to the intracellular space, resulting in brain edema and seizures.
- Cardiac arrhythmias: Potassium imbalances caused past dehydration tin affect muscles and cause life-threatening cardiac arrhythmias, fatigue, weakness, and musculus breakdown.
- Heatstroke: During practice or while working in a hot environment, fluid intake is recommended to avoid oestrus exhaustion or even heatstroke.
- Kidney failure: Possible causes of kidney injury include hypovolemic shock with low blood supply to the kidneys, acidosis due to hypovolemia, musculus breakup, and electrolyte disturbances.
- Thrombosis: Increased blood viscosity from dehydration will lead to venous thrombosis. Patients may present with DVT, portal vein thrombosis, or pancreatitis. Fever will also increase thrombosis take a chance and limit water intake.
- Blackout and death: Low blood pressure in severe aridity will decrease blood supply to the encephalon and could cause coma or death, particularly in elderly patients.
Prevention of Dehydration
Adequate hydration is recommended during all activities to prevent dehydration. H2o intake is primal to replacing fluid lost during exercise, in hot weather, during hospitalization, and in elderly patients with dumb thirst awareness.
Hospitalized patients should exist advisedly monitored for water intake and total fluid output for early on detection of any fluid imbalances.
Children with vomiting and diarrhea should not be given plain h2o to replace fluid lost as this could pb to hyponatremia and water intoxication.
Intravenous fluids can be used for fluid replacement in unconscious patients with astringent aridity while apparently water, sports drinks with electrolytes, and oral rehydration solutions are used for the prevention and treatment of mild dehydration. Electrolyte monitoring is mandatory for patients using diuretics for prolonged periods.
Treatment of Aridity
Treatment approaches vary according to patient age and severity of dehydration.
Handling of the crusade should always be considered, forth with the treatment of symptoms and fluid replacement. Urine output should be monitored in hospitalized patients as an indicator of treatment efficacy and renal role recovery.
In severe dehydration, restoration of the blood book is the main goal and is achieved with a fluid bolus of 20 mL/kg isotonic saline or Ringer's lactate. Adults can utilise oral fluids if they are conscious and able to drink, otherwise, intravenous fluids should be used. Correction of electrolyte abnormalities should follow.
Infants and children with aridity
Children are vulnerable to the effects of dehydration. Water impecuniousness tin complicate gastroenteritis or fever and can lead to severe dehydration, with neurological manifestations and electrolyte imbalances.
Treatment options include fluid replacement orally if the child is witting and able to drink. Water, fluids, and an oral rehydration solution can be used. In severe cases, intravenous fluids should be used.
Breastfeeding and a normal nutrition should be continued, as long equally the treatment with fluid replacement prevents weight loss or developmental delays in infants.
Treatment of isonatremic dehydration
A fluid bolus should be given to restore the blood volume according to severity, followed by maintenance therapy with 0.9% normal saline; 20 mL/kg of isotonic sodium or Ringer's lactate is given to restore hydration. Oral intake should be encouraged as early as possible.
Treatment of hyponatremia
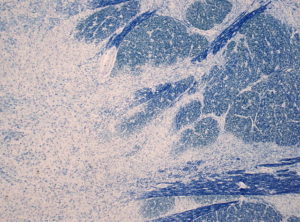
Image: "Loss of myelinated fibers at the basis pontis in the brainstem (Luxol-Fast blue stain)" by Jensflorian – Ain work. License: CC BY-SA three.0
Patients may present with astute cognitive edema. Early steps should include stabilization of the patient, securing of the airway, and maintenance of breathing and circulation.
In severe astute cases involving seizures and coma, management of hyponatremia is accomplished with 3% hypertonic saline. Correction of hyponatremia should start at a rate of 4–six mEq/L/60 minutes.
In chronic hyponatremia, correction of sodium concentration should be done using 0.9% normal saline at a rate of 10–12 mEq/L/day during the first 2 days. The rapid correction of hyponatremia will lead to central pontine myelinolysis, resulting in permanent injury to the brain stalk, quadriplegia, and cranial nerve paralysis.
To summate the sodium deficit:
Sodium deficit = (normal sodium level – serum level) × volume of distribution × weight
Treatment of hypernatremia
The first pace in treating hypernatremia is volume restoration with isotonic saline or Ringer's lactate.
Post-obit this, a slow correction of the hypernatremia at a charge per unit of 10 mEq/L/24hours is required to avoid complications (cerebral edema and death). five% dextrose in 0.9% sodium chloride tin can be used with frequent monitoring of the serum sodium every iv hours.
Hyperglycemia and hypocalcemia occasionally follow hypernatremic aridity; thus, serum glucose and calcium levels should exist monitored closely.
Note: Antidiarrheal agents, routine antibiotics, and antiemetics should be avoided in this situation every bit they may worsen the status.
soulierecompearid.blogspot.com
Source: https://www.lecturio.com/magazine/dehydration/
Belum ada Komentar untuk "Dehydration Can Be Described as a Water Loss"
Posting Komentar